Abstract
Introduction
Multiple myeloma (MM) patients have an increased risk of severe coronavirus disease 2019 (COVID-19) when infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Monoclonal gammopathy of undetermined significance (MGUS) precedes MM and related disorders and affects 4.2% of the general population over the age of 50 years. MM and MGUS are associated with immune dysfunction that is believed to contribute to the development of severe COVID-19. Currently, no systematic data on MGUS and COVID-19 have been published. We conducted a large population-based cohort study to evaluate whether MGUS was associated with SARS-CoV-2 infection and the development of severe COVID-19.
Methods
Data on all SARS-CoV-2 test results and COVID-19 severity was acquired from the COVID-19 Outpatient Clinic at Landspitali - The National University Hospital of Iceland. The first case of COVID-19 in Iceland was diagnosed on February 28 th, 2020. Since then, the Icelandic authorities have followed an aggressive strategy of SARS-CoV-2 testing and contact tracing. All SARS-CoV-2-positive individuals were immediately contacted and those with active infection were enrolled into telehealth monitoring consisting of repeated standardized interviews conducted by a nurse or physician. If clinical deterioration was detected, patients were assessed in person at the COVID-19 Outpatient Clinic and admitted if needed.
Study participants were included from the Iceland Screens Treats or Prevents Multiple Myeloma study (iStopMM). The study is an ongoing population-based screening study for MGUS and randomized trial of follow-up strategies. Out of the 148,708 Icelanders who were born 1976 and earlier and were alive on September 9 th 2016, 80,759 (54%) provided informed consent for study participation and 75,422 (94%) of those provided a blood sample for MGUS screening by serum protein electrophoresis (SPEP) and free light chain (FLC) assay. MGUS was determined by current criteria using SPEP and FLC assay data. Individuals who had died, been diagnosed with MM and related disorders, or were undergoing treatment for smoldering MM prior to February 28 th were excluded.
First, the association of MGUS and testing positive for SARS-CoV-2 was evaluated. We used a test negative design and included participants who had been tested at least once for SARS-CoV-2 between February 28 th and December 31 st, 2020. The association of MGUS and a positive test for SARS-CoV-2 was assessed using logistic regression, adjusted for sex and age.
Next, the association of MGUS and severe COVID-19 was evaluated. Those who tested positive for SARS-CoV-2 were included unless they were hospitalized or living in a nursing home at diagnosis. Participants were followed until discharge from telehealth monitoring or until considered having severe COVID-19. Severe COVID-19 was defined as the composite outcome of the need for outpatient visit or hospital admission and death and as the composite outcome of hospital admission and death. Logistic regression was then performed adjusting for sex and age.
Results
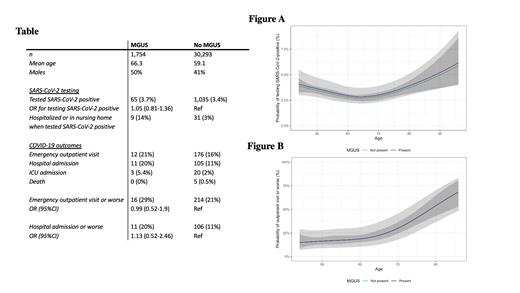
Of the 75,422 individuals screened for MGUS, 32,047 (42%) were tested for SARS-CoV-2 during the study period of whom 1,754 had MGUS (5.5%). Those with MGUS were older (mean age 66.3 vs 59.1 p<0.001) and more likely to be male (50% vs 41% p<0.001). In total, 1,100 (3.4%) of the participants tested positive for SARS-CoV-2 of whom 65 had MGUS. After adjusting for sex and age, MGUS was not found to be associated with testing positive for SARS-CoV-2 (odds ratio (OR): 1.05; 95% confidence interval (CI): 0.81-1.36; p=0.72; Table; Figure A).
Of those who tested positive for SARS-CoV-2, a total of 230 had the composite outcome of requiring an outpatient visit or hospital admission, and death, and 117 had the composite outcome of hospital admission and death. After adjusting for age and sex, MGUS was not found to be associated with either endpoint (OR: 0.99; 95%CI: 0.52-1.91; p=0.99 and OR: 1.13; 95%CI: 0.52-2.46; p=0.76; Table; Figure B)
Conclusions:
In this large population-based study that included 75,422 individuals screened for MGUS, we did not find MGUS to be associated with SARS-CoV-2 susceptibility or COVID-19 severity. This is contrary to MM which is preceded by MGUS. These findings suggest that immunosuppression in MGUS differs significantly from that of MM and are important since they can inform management and recommendations for individuals with MGUS.
Kampanis: The Binding Site: Current Employment. Hultcrantz: Intellisphere LLC: Consultancy; Daiichi Sankyo: Research Funding; Curio Science LLC: Consultancy; Amgen: Research Funding; GlaxoSmithKline: Membership on an entity's Board of Directors or advisory committees, Research Funding. Durie: Amgen, Celgene/Bristol-Myers Squibb, Janssen, and Takeda: Consultancy; Amgen: Other: fees from non-CME/CE services . Harding: The Binding Site: Current Employment, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties. Landgren: Amgen: Honoraria; Janssen: Honoraria; Celgene: Research Funding; Janssen: Other: IDMC; Janssen: Research Funding; Takeda: Other: IDMC; Amgen: Research Funding; GSK: Honoraria. Kristinsson: Amgen: Research Funding; Celgene: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal